Do you know cervical cancer is the 4th most common form of cancer and female cancer-related deaths worldwide? The WHO reports an estimated 528,000 cervical cancer cases in 2012 followed by 266,000 deaths which accounted for 8% of total cancer cases and total cancer deaths.
Second only to breast cancer, this is the most common female-centric cancer accounting about 7.9% of all female cancers. 90% of the world’s cervical cancer deaths have been reported from developing and underdeveloped nations. [http://www.who.int]
The American Cancer Society reports:
- In 2018, about 4170 women in the US are estimated to die from cervical cancer.
- About 13,240 new cases of invasive cervical cancer will be diagnosed by this year. [cancer.org]
In the UK, the rate of cervical cancer incidences is projected to rise by 43% in 2014-35. There would be an estimated 17 cervical cancer cases per 100,000 women in 2035. [www.cancerresearchuk.org]
Cervical cancer once considered one of the common causes of cancer-related deaths in American women, hasn’t fully loosened its deadly claws although the death rates from this disease fell sharply past few years. Thanks to the advanced screening procedures enabling early detection of changes in the cervix but the situation hasn’t changed much for women residing in underserved or backward areas.
Few quick facts:
- Cervical cancer, among all gynecological cancers, is the easiest to prevent.
- All cases of stage 0 of cervical cancer or Carcinoma in situ (CIS) can be cured though chances of relapse exist.
- The estimated 5- year survival rate can be about 93% [depending on the cancer stage]
- Regular screening and vaccination can effectively prevent cervical cancer.
- This cancer is rare in women who take regular screening tests.
- The high mortality rate in economically backward nations can be reduced through a comprehensive approach to prevention, proper screening, timely diagnosis and treatment.
- Along with commonly adopted diagnostics and treatment modalities, analysis of The Cancer Genome Atlas (TCGA) may advance cervical cancer treatment through personalized genome-targeted approach.
[https://www.cancer.org], [[http://www.who.int]
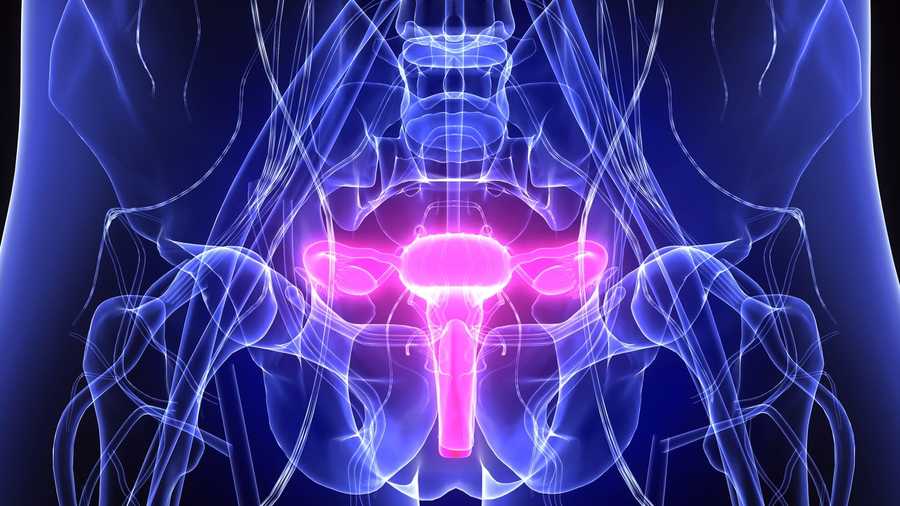
Cervical cancer – site of occurrence:
Anomalous growth of cells is observed in the cervix, the small extended part of the uterus of the female reproductive system connected to the birth canal, which gradually invades surrounding tissues and organs. The cancer develops slowly from the precancerous stage (dysplasia) for over 10-20 years.
Common forms of cervical cancer:
Squamous cell carcinoma: Accounts for almost 90% of cervical cancer cases.
Adenocarcinoma: Accounts for about 10% cervical cancer cases. [https://en.wikipedia.org]
A small fraction of cervical cancer cases often is Mixed Carcinoma having features of both the above types of carcinoma.
Symptoms:
Cervical cancer at the initial stages normally does not show any symptoms. This is the reason why it gets detected later in many women making it almost untreatable ultimately leading to death. Typical symptoms are:
- Abnormal vaginal bleeding. It can be occasional in between menstrual periods, after sex or after menopause.
- Unusual heavy menstrual flow.
- Pain during sex.
- Usual vaginal discharge and odor.
- Pelvic pain.
If the cancer invades surrounding tissues, the symptoms can be more like:
- Painful urination followed by blood in urine
- Fatigue, loss of weight and appetite
- Diarrhea or pain and rectal bleeding during defecation
- Swollen abdomen, feeling of nausea and vomiting
- Mild backache and swollen limbs
Cause:
90% of cervical cancer cases are due to Human Papillomavirus infection (HPV), which is very common. The American Centers for Disease Control and Prevention (CDC) reports about 6 million HPV infections every year. 20 million people already have it and more than 50% sexually active adults are likely to acquire this infection at some point of their life. [https://www.healthline.com/]
- All people with HPV infection do not develop cervical cancer. The infection gets eliminated on its own within 1 or 2 years the reason for which is still not understood. [https://www.healthline.com/]
- Among 150-200 types of HPV known, 15 types fall into high-risk category, 3 into probable high-risk category and 12 into low risk category.
- Of the high-risk HPV category, HPV 16 & 18 account for 75% and HPV 31& 45 account for 10% of cervical cancer cases respectively. [https://en.wikipedia.org]
How HPV infection spreads?
HPV is highly contagious. Most people even don’t know that they are carrying HPV. It spreads fast through direct skin to skin contact attacking the moist lining of the body.
Therefore, HPV infection normally spreads through:
- Unprotected sexual intercourse especially among women having multiple sex partners.
- Any type of sex whether it is vaginal, oral or anal.
- Women who get into sexual activity at a very young age.
Who are at risk of getting cervical cancer?
Women of all age carry the risk of developing cervical cancer but the risk increases with age.
- Mostly women aged between 35 and 44 years.
- More than 15% of cervical cancer cases have been observed in women above 65 years of age.
- Hispanic women in the US. [https://www.cancer.org]
Other risk factors include:
- Experiencing first intercourse at a very early age.
- Sexually active
- Multiple sex partners.
- Having sex with an HPV infected person
- A medical history of STIs (sexually transmitted infections)
- Not conducting regular Pap tests
- HIV infection.
- Full-term pregnancy before 17 years of age.
- Multiple pregnancies more than 3 times.
- More than 5 years usage of oral contraceptives
- Smoking
- Overweight/obesity
- Chlamydia infection
- Family history of cervical cancer
- Exposure to hormonal drug diethylstilbestrol (DES) during the fetal stage. These are exceptional cases where cancers are not caused by HPV.
Diagnosis:
Pap test is normally done as a screening test, but it often gives false negatives in about 50% cervical cancer cases. Confirmation of precancerous and cancerous stage can be obtained through biopsy only which is done through Colposcopy. Cervical biopsies diagnose Cervical Intraepithelial neoplasia (precancerous lesions) with proper grading, a high potential factor which later develops into cancer.
Ultrasound, CT scan and MRI can be done to rule out possibilities of other ailments before a biopsy. Further diagnostic procedures include LEEP (Loop Electrical Excision Procedure) and Cervical Conization mostly in severe cases.
Treatment:
Cervical cancer treatment is based on its staging, that is, its size, extent of invasion and spread. Treatment modalities include:
- Surgery involving Hysterectomy with complete removal of cervix
- Radiation Therapy
- Chemotherapy
- Targeted therapy
Earlier stages of cervical cancer are treated with surgery or radiation or these may be combined with chemotherapy.
For treating later stages, radiation is often combined with chemotherapy.
Chemotherapy is mainly applied in the advanced stages.
Advanced treatment approach with genomics:
According to National Foundation for Cancer Research, research on genomics also helps to attack cervical cancer with a personalized approach. [https://www.nfcr.org].
Researchers of The Cancer Genome Atlas (TCGA) network are hopeful to get new insights into cervical cancer treatment by adopting different therapeutic approaches. The study involving genome analysis of 178 primary cervical cancers was supported by the National Cancer Institute (NCI) and National Human Genome Research Institute (NHGRI). The results were published in the Nature journal on January’17.
Women beyond the recommended age of vaccination but with a probability to develop cervical cancer in future are likely to benefit from this genome-targeted treatment approach where new drugs targeting specific cervical cancer genomes along with HPV would be more effective. [https://www.nih.gov]
Important tips to prevent cervical cancer:
This gynecological cancer is easiest to prevent through regular screening tests, follow ups and little bit of lifestyle modifications. Prevention starts from the early pre-cancerous stage before it turns out to be cancerous.
Total abstinence from sex may be the best way to prevent cervical cancer-inducing HPV infection but this is not practically applicable. All sexually active women can be exposed to HPV infection.
Therefore, preventive measures include the following:
- Getting HPV vaccination at an early age of 11-12 years before the first intercourse. It can be given earlier at the age of 9-10 years too. Those missing the early vaccination can get the catch-up vaccine till 18 years of age. Other women aged 19-26 years may also get the vaccination. [https://preventcancer.org]
- All women should go for screening tests from 21 years of age even after vaccination.
- Women aged from 21-29 should go for regular Pap smear test every 3 years. In this test, cells collected from the cervix are studied under a microscope to detect any undesirable changes.
- From 30 years of age, women should have a combined screening test of Pap Smear and HPV every 5 years which should continue until the age of 65.
- However, the best option for women aged between 30 and 65 to go for only Pap smear test every 3 years.
- Those with a compromised immune system due to HIV infection, organ transplant, long-term steroid use or exposed to DES (diethylstilbestrol) in fetal stage may be required frequent screening as guided by the medical care team. [https://www.cancer.org]
Preventive lifestyle measures to reduce the risk of cervical cancer:
- Practice safe sex using barriers like spermicidal gels, condoms, dental barriers etc.
- Limit your sexual partner to one.
- Quit smoking
- Follow a nutritious diet containing high quantities of Vitamin A, B12, Vitamin C, E and beta carotene
HPV vaccination – When and how?
The sooner you get safer you are. Sexually active women may get vaccinated later but it would be less effective. HPV vaccination is absolutely safe and clinical trials have proved that it provides almost 100% protection from cervical pre-cancers and genital warts.
Shots of HPV vaccine are expensive. One can avail this vaccine through government-run immunization programs where the vaccine is available either free or carry a minimum cost.
According to the latest CDC recommendations in 2016, younger adolescents should get 2 doses of vaccination before their 15th birthday. Older adolescents after 15 years of age need 3 doses of HPV vaccination. [https://www.cdc.gov]
- Women above 26 years of age are not recommended for HPV vaccination. Regular screening is the best way to prevent cervical cancer.
- HPV vaccine is not recommended for pregnant women.
- Women should continue the screening tests even after completing the recommended vaccine dosages since they do NOT give protection for all types of cervical cancers.
- HPV vaccination is most effective before getting exposed to HPV.
- The vaccine does not give protection from all types of HPV. It does not protect from other STIs.
- Cervarix, Gardasil and Gardasil 9 are the available HPV vaccinations which have undergone extensive safety tests before approved by FDA.
- This vaccination is also effective for boys and young men aged 9-26 years.
Awareness is the key to prevent cervical cancer:
Sheer lack of awareness is pushing millions of women towards dreadful consequences of cervical cancer. Adequate health literacy along with regular screening tests conducted in developed nations has drastically cut the cervical cancer mortality rates, but the situation remains gloomy in the developing and economically backward nations.
Death from cervical cancer is a disgrace to the society when this disease can be easily prevented just by generating mass awareness. Ground breaking medical advancements will not fetch any substantial benefits unless the awareness regarding the cause and prevention of this disease among the population is seriously considered.

